Vaginal and Vulvar Problems and Best Care Practices
Every woman experiences some pain and discomfort in their vulva or vagina at some point. Understanding what may be the cause and when to call your Moreland OB-GYN provider is important to know.
Below, we outline some of the most common vaginal and vulvar problems and disorders and also talk through how to care for your vagina and vulva appropriately.
First, let’s start by understanding the difference between your vulva and vagina. Knowing the correct terms for our body parts empowers us to take full ownership of them. It also makes it easier to discuss issues with others, like your doctor, partner, or your daughters.
.png?width=350&name=Untitled%20design%20(13).png)
Vulva and Vagina
You may hear "vulva" and "vagina" used interchangeably, but they are very different and distinct.
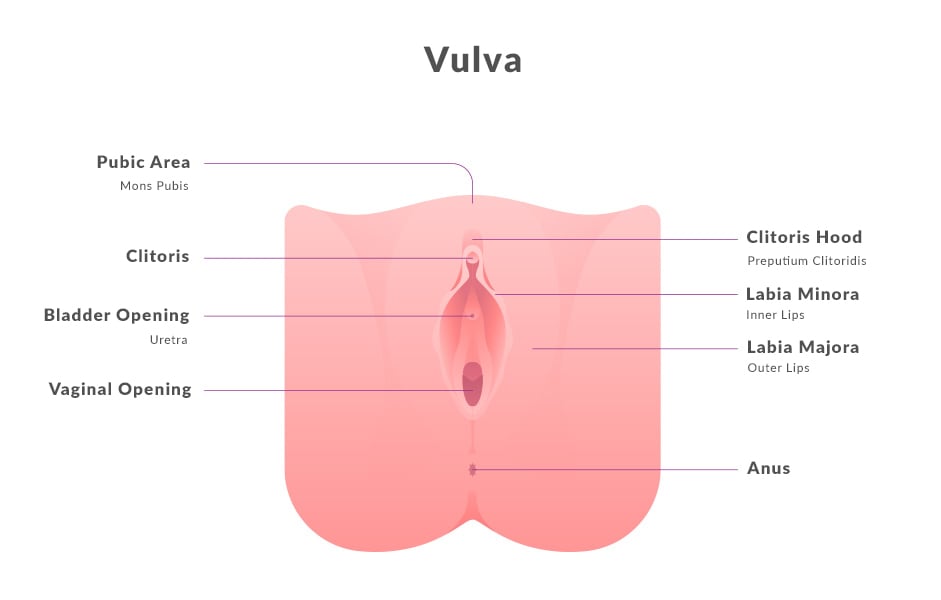
The Vulva
The vulva is the external female genital area, which includes your labia minora, labia majora, clitoris, and openings to the urethra and vagina. The vulva protects the female sex organs, urinary opening and vagina, and is the center of much of a woman’s sexual response. No two are alike, but they all have the following features in common:
- The labia are the folds of skin around your vaginal opening. The fleshy outer set, called labia majora, surrounds the labia minora, which starts at the tip of your clitoris and ends under the opening of your vagina.
- The tip of the clitoris is located at the top of your vulva, where the labia minora meet. The clitoris extends inside the body, back and down on both sides of the vagina. Pleasure is the clitoris’ normal physiological function.
- The urethral opening sits just below your clitoris and is the opening you urinate from.
- The vaginal opening, below the urethral opening, is the gateway to your internal genitalia.
- The Bartholin glands are located on either side of the vaginal opening. They release a fluid that helps with lubrication during sexual intercourse.
- The anus is the opening to your rectum.
- The perineum is the external skin between the vaginal opening and the anus. It’s not part of the vulva but may be involved in vulvar skin problems.
- The mons pubis is the fleshy mound above your vulva that cushions your pubic bone.
The Vagina.png?width=350&name=Untitled%20design%20(12).png)
The vagina is an internal, muscular canal that:
- Extends from the vulva and connects the uterus to the vulva
- Funnels your menstrual flow
- Allows for penetration during sex
- Provides a pathway for childbirth
The vagina is a warm, dark space with multiple secretory glands. It has its own delicately balanced ecosystem. Good bacteria help keep your vagina healthy by producing lactic acid, hydrogen peroxide and other substances to keep harmful bacteria at bay. They help maintain your vaginal pH levels by keeping it acidic to ward off the overgrowth of yeast and other harmful bacteria.
Common Vaginal Problems
Vaginal Odors
Your vagina comes complete with its own unique, odor-producing bacterial flora. You may not notice your vaginal odor, and even when you pick up a scent, it may be due to menstrual blood, sexual intercourse or a host of other normal odor-producing reasons.
But if you notice a strong, fishy odor—especially if it’s accompanied by itching or irritation —it may indicate something more serious.
Unusual Vaginal Discharge
The amount of vaginal discharge you experience changes with your menstrual cycle. If you are experiencing clear discharge with either no scent or a light musky odor, you are likely ovulating. This discharge is normal. However, other types of discharge typically signal an infection and should be checked out by your provider.
Vaginal Infections
When your normal pH levels are upset, a vaginal infection may occur. The three most common types of vaginal infections are discussed below.
- Bacterial Vaginosis (BV) is a bacterial infection that occurs when your healthy lactobacilli are outnumbered by unhealthy bacteria, causing an imbalance. Symptoms include thin gray, yellow or green colored vaginal discharge with a strong fishy smell and minor itching or burning when urinating. BV is diagnosed by your OBGYN and is treated with an antibiotic.
- Yeast infections are caused by an overgrowth of a fungus, called Candida, which generally exists in small amounts in the mouth, throat, gut, and vagina. Factors that can promote yeast to over-produce include antibiotics, pregnancy, diabetes or a weakened immune system. Symptoms may include vaginal and vulvar itching, redness and irritation of the vulvar skin, and thick, white vaginal discharge. Yeast infections are treatable with antifungal medication.
- Trichomoniasis is a sexually transmitted infection caused by a parasite. Women with trichomoniasis may notice a clear, white, yellowish or greenish vaginal discharge; a heavy fishy vaginal odor; genital itching; burning, redness, or soreness; and urinary discomfort. Trichomoniasis is diagnosed by your OBGYN and treated with antibiotics.
A forgotten tampon (it happens more than you realize) could also cause a vaginal infection. Symptoms of a forgotten tampon include a putrid-smelling vaginal discharge that’s yellow, green, pink, gray, or brown. You may also experience additional symptoms, including fever, vaginal itching, pain urinating, pain around your pelvis or abdomen, redness around the genital area and vaginal swelling. If you cannot easily retrieve the tampon and are experiencing these symptoms,
call your Moreland OB-GYN provider.
If you are pregnant and have symptoms of a vaginal infection, schedule an appointment with your Moreland OB-GYN provider. Conditions like bacterial vaginosis could affect your pregnancy.
Vaginal Dryness
Vaginal dryness occurs when the vaginal tissues do not produce sufficient natural lubrication, leading to discomfort and potential complications. Vaginal dryness can be caused by various factors, including a drop in estrogen levels (such as during menopause or breastfeeding), certain medications and birth control, stress, lack of arousal and medical conditions. Vaginal dryness symptoms may include itching, burning sensation, pain during intercourse and general discomfort. While menopause is a common cause of vaginal dryness, it’s important to know it can occur in women of any age. Treatments for vaginal dryness are available by prescription, such as hormone replacement therapy and over-the-counter lubricants and moisturizers.

Common Vulvar Problems
The vulva skin can often be more sensitive compared to the skin on the rest of the body and is subject to a range of vulvar skin problems. Some skin disorders that affect the vulva include:
- Folliculitis. Folliculitis appears as small, red, and sometimes painful bumps caused by bacteria that infect a hair follicle. It can occur on the labia majora. These painful bumps can appear because of shaving, waxing or friction. Folliculitis often goes away by itself. Attention to hygiene, wearing loose clothing and warm compresses applied to the area can help speed up the healing process. See your healthcare provider if the bumps do not go away or they get bigger. You may need additional treatment.
- Contact dermatitis. Contact dermatitis is caused by skin irritation by things such as soaps, fabrics or perfumes. Signs and symptoms can include extreme itching, rawness, stinging, burning and pain. Treatment involves avoiding the source of irritation and stopping the itching so the skin can heal. Ice packs or cold compresses can reduce irritation. A thin layer of plain petroleum jelly can be applied to protect the skin. Medication, such as a topical steroid cream or ointment, may be needed for severe cases.
.png?width=350&name=Untitled%20design%20(14).png)
- Bartholin gland cysts. If the Bartholin glands become blocked, a cyst can form, causing a swollen bump near the opening of the vagina. Bartholin gland cysts usually are not painful unless they become infected. If this occurs, an abscess can form. If your cyst is not causing pain, it can be treated at home by sitting in a warm, shallow bath or applying a warm compress. If an abscess has formed, treatment involves draining the cyst in a health care provider’s office.
- Lichen simplex chronicus. Lichen simplex chronicus may result from contact dermatitis or other skin disorder that has been present for a long time. Thickened, scaly areas called “plaques” appear on the vulvar skin. These plaques cause intense itching that may interfere with sleep. Treatment involves stopping the “itch-scratch” cycle so that the skin can heal. Steroid creams often are used for this purpose. The underlying condition should be treated as well.
- Lichen sclerosus. Lichen sclerosus is a skin disorder that can cause itching, burning, pain during sex, and tears in the skin. The vulvar skin may appear thin, white, and crinkled. White bumps may be present with dark purple coloring. A steroid cream or ointment is used to treat lichen sclerosus. Lichen sclerosus does not affect the vaginal canal.
- Lichen planus. Lichen planus is a skin disorder that most commonly occurs on the mucous membranes of the mouth. Occasionally, it also affects the skin of the vulva and vaginal canal. Itching, soreness, burning, and abnormal discharge may occur. The appearance of lichen planus is varied. There may be white streaks on the vulvar skin, or the entire surface may be white. There may be bumps that are dark pink. Treatment of lichen planus may include medicated creams or ointments, vaginal tablets, prescription pills, or injections. This condition is difficult to treat and usually involves long-term treatment and follow-up.
Vulvodynia
Vulvodynia means “vulvar pain” and is a chronic condition characterized by persistent, unexplained pain and discomfort in the vulvar area. The pain can occur when the area is touched (provoked), or without touch (unprovoked).
There are two types of vulvodynia: generalized and localized.
- Generalized vulvodynia: Pain occurs over a large area of the vulva.
- Localized vulvodynia: Pain is felt in a smaller area, such as the vestibule (the vaginal opening).
Vulvodynia is a complex condition with no clear identifiable cause, making diagnosis and treatment challenging. Symptoms of vulvodynia can vary among individuals but often include burning, stinging, or rawness in the vulvar area. The pain may be constant or sporadic and can significantly impact daily activities, including sexual intercourse. While the exact cause is unknown, factors such as nerve abnormalities, hormonal changes, muscle dysfunction, and previous vaginal infections or injuries may contribute to its development.
Treatment approaches for vulvodynia typically involve a multidisciplinary approach, including medication, topical creams, physical therapy, counseling, and lifestyle modifications. It's important for individuals experiencing symptoms to seek medical advice for proper diagnosis and to develop a personalized treatment plan.
At Moreland OB-GYN, our caring providers will take the time to understand what may be causing your vaginal dryness and recommend the best treatment plan so you can live your healthiest and happiest life. Schedule an appointment today!
Gentle Care for Your Vagina and Vulva
Cleanliness and comfort can help alleviate vulvar and vaginal issues. The good news is, vulva and vaginal care is pretty simple and doesn’t involve drastic lifestyle changes.
Cleaning your Vulva and Vagina
.png?width=350&name=Untitled%20design%20(15).png) Wash your vulva daily with warm water —soap is optional, but use a gentle, fragrance-free soap like Dove-Hypoallergenic, Neutrogena, Basis, or Pears. Use your fingers instead of a washcloth.
Wash your vulva daily with warm water —soap is optional, but use a gentle, fragrance-free soap like Dove-Hypoallergenic, Neutrogena, Basis, or Pears. Use your fingers instead of a washcloth.
- Do not wash inside your vagina. The vagina cleans itself with discharge to maintain a consistent pH balance.
- Avoid using any vaginal scrubs, scented soaps and douching. Using these products can throw off your natural pH balance and increase the chance of infection.
- After you go to the bathroom, wipe from the front to the back. Doing the reverse could transfer bacteria to the urethra and cause a urinary tract infection.
Good Practices for Caring for Your Vulva and Vagina
Clothing
Choose clothing that will ensure your vulvovaginal area can breathe easily and stay dry. Moisture can promote the growth of bacteria, which can lead to a yeast infection.
- Wear cotton underwear. Cotton offers breathability and makes it more difficult for smell-producing bacteria to build up. Avoid wearing thongs because they can collect fecal matter that can reach the vagina and cause infections.
- Avoid tight-fitting clothing.
- Change your clothes and underwear after working out.
- Avoid wearing a damp swimsuit all day.
- If you experience heavy vaginal discharge, change your underwear twice a day.
- At night, reduce sweat being trapped around the vulva by forgoing underwear.
A few more tips regarding good vulvovaginal health
- Avoid scented tampons, pads, and liners.
- During your period, change your tampon 4 to 5 times a day. That goes for pads and liners, as well.
- Wash or wipe the area regularly during your period.
- Consuming probiotics like yogurt can help prevent yeast infections and reduce vaginal odor by keeping your vagina’s pH levels in order.
- Stay well-hydrated because it helps to keep bacterial overgrowth and stress-related sweat in check.
- Perform a regular vulvar self-exam, which can help you become aware of the normal appearance of your vulva and help you identify any abnormalities that may indicate infection, vulvar cancer, or vulvar skin condition.

When To Call Your OBGYN Provider
See your Moreland OB-GYN provider annually for your wellness visit and in between if you have any concerns or questions about the health of your vulva and vagina.
Pay attention to unusual vaginal discharge and odors, especially when those symptoms are accompanied by:
- Fever
- Bleeding not associated with your period
- Itching
- Burning
- Vaginal swelling
- Genital rash or redness
If you notice any unusual vaginal symptoms or changes in your vulvar skin, contact your doctor and schedule an appointment.
Moreland OB-GYN is proud to be a leading women’s healthcare provider, serving outstanding care at our seven locations across southeastern Wisconsin. We work with every patient to deliver compassionate patient care focused on shared decision-making and an exceptional patient experience.
We hope you'll contact us to answer any questions or concerns you have surrounding vaginal and vulvar health. Our caring team of providers will take the time to listen and supply the resources and information you need to live your best and healthiest life.
Learn more about our services and contact us online to request an appointment.
.png?width=350&name=Untitled%20design%20(13).png)
.png?width=350&name=Untitled%20design%20(12).png)
.png?width=350&name=Untitled%20design%20(14).png)
.png?width=350&name=Untitled%20design%20(15).png) Wash your vulva daily with warm water —soap is optional, but use a gentle, fragrance-free soap like Dove-Hypoallergenic, Neutrogena, Basis, or Pears. Use your fingers instead of a washcloth.
Wash your vulva daily with warm water —soap is optional, but use a gentle, fragrance-free soap like Dove-Hypoallergenic, Neutrogena, Basis, or Pears. Use your fingers instead of a washcloth.