Osteoporosis vs. osteoarthritis— they sound very similar, but what’s the difference? They are both common bone conditions that occur with aging.
In this post, we’ll discuss the difference between osteoporosis and osteoarthritis along with a review of:
- Risk factors
- Symptoms
- Treatment options
As you review the information below, please feel free to reach out to your Moreland provider with any questions and concerns about osteoporosis and osteoarthritis.
Osteoporosis vs. Osteoarthritis Overview
Before we can compare these two conditions, it’s important to first explain the specifics of each.
What is Osteoporosis?
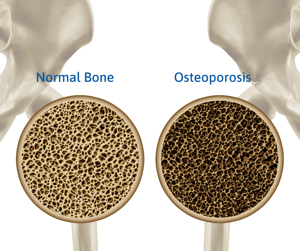
Osteoporosis affects the interior structure of bones. In healthy bones, tissue constantly reabsorbs old cells and grows new tissue to maintain strength and density. Our bodies do this very well in our youth and into our 20s when we reach peak bone mass.
As we age, however, this process slows. Osteoporosis occurs when bone loss outpaces bone growth. Bones become more porous, which weakens their integrity and makes them more at risk for fractures. Wrist, hip, and spine fractures are common among women with osteoporosis.
According to the CDC, osteoporosis affects nearly 1 in 5 women over age 50 in the US.
Learn more about osteoporosis now in our blog: Osteoporosis Guidelines: Symptoms, Doctors, Treatments, and More
What is Osteoarthritis?

Osteoarthritis affects bones’ external structure. It is a degenerative joint disease caused by overuse of a joint, where cartilage supporting a joint wears away over time, allowing the bones to rub together, causing pain, stiffness, and swelling.
The likelihood of developing osteoarthritis increases as we age. It can reduce an individual’s functionality, creating disabilities. The neck, hands, back, hips, knees, and big toes are common targets of this degenerative joint disease.
The US Bone and Joint Initiative estimates more than 3 in 5 individuals with osteoarthritis are women
A Review of Risk Factors
Both osteoporosis and osteoarthritis come with risk factors, some that you can control, and others you cannot.
Osteoporosis Risk Factors
Osteoporosis risk factors outside of your control include:
- Gender: Women are four (4) times more likely to develop osteoporosis than men. The decline of estrogen that comes with menopause causes greater risk because estrogen is important to build and maintain strong bones.
- Age: As we age, the likelihood of osteoporosis increases.
- Genetics: Having a parent or sibling with osteoporosis—especially if they suffered a hip fracture—puts you at greater risk.
- Race: If you’re of Caucasian or Asian descent, you’re at the greatest risk of developing osteoporosis.
- Body frame size/weight: Small or underweight body frames may have less bone mass and pose a higher risk for developing osteoporosis.
- Other health conditions: Calcium regulation or bone metabolism can be disrupted by diabetes or hyperthyroidism, increasing the risk of osteoporosis. Celiac disease, inflammatory bowel disease, kidney disease, liver disease, and cancer are other health conditions that come with a greater risk for osteoporosis.
Osteoporosis risk factors you can control include:
- Alcohol consumption: Consuming more than two (2) alcoholic drinks a day increases the likelihood of osteoporosis.
- Sedentary lifestyle: Sedentary individuals are at greater risk than active individuals.
- Diet: Low consumption of calcium and Vitamin D increases risk. Tally your daily calcium consumption with this worksheet.
- Medications: Long-term use of steroids interferes with bone-building, causing greater risk.
- History of smoking: According to the American Academy of Orthopaedic Surgeons, smoking:
- Increases the risk of osteoporosis. Elderly smokers are 30% to 40% more likely to break their hips than elderly non-smokers.
- Weakens bones by reducing blood supply to bones and slows the production of bone-forming cells.
- Interferes with the absorption of calcium.
- Breaks down estrogen in the body more quickly.
Osteoarthritis Risk Factors
Osteoarthritis also comes with risk factors that are within and outside of our control.
 Osteoarthritis risk factors beyond our control include:
Osteoarthritis risk factors beyond our control include:
- Age: As we age, the risk of osteoarthritis increases.
- Gender: Women, especially those over 50 years old, are at greater risk of developing osteoarthritis. Estrogen is important for building and maintaining healthy bone; menopause creates a deficiency of estrogen, increasing the risk of osteoporosis.
- Genetics: Having family members with osteoarthritis increases your chances of developing the condition. According to the CDC, people with osteoarthritis in their hands are also more likely to develop osteoarthritis in their knees.
- Race: Certain Asian populations are less likely to develop osteoarthritis.
- Joint injuries: Old joint injuries can increase your risk of developing osteoarthritis.
- Bone deformities: Having malformed joints or defective cartilage can increase the risk for osteoarthritis.
- Metabolic diseases, including diabetes and hemochromatosis (an excess of iron in the body), can elevate risk.
Other osteoarthritis risk factors within our control include:
- Obesity: Excess body weight stresses your weight-bearing joints—your hips and knees. Also, fat cells produce and release proteins into your body that cause inflammation around joints.
- Sedentary lifestyle: Cartilage can shrink due to a lack of exercise, causing stress on your joints and putting you at greater risk of developing osteoarthritis.
A Review of Symptoms
Both osteoporosis and osteoarthritis develop gradually over time, but symptoms present themselves differently.
Osteoporosis Symptoms
Osteoporosis is sometimes called a silent disease. Many individuals don’t realize they have it until they experience a sudden, surprising bone fracture.
Osteoporosis symptoms include:
- Lower back pain, caused by fractured vertebrae or collapsed discs
- A decrease in height of an inch or more
- Stooped posture
- Shortness of breath, due to a decrease in lung capacity caused by spinal collapse
Learn more about osteoporosis now.
Osteoarthritis Symptoms
Osteoarthritis symptoms are less subtle than those of osteoporosis. They include:
- Pain around the affected joints during movement
- Stiffness after sleeping or being otherwise inactive
- Decreased flexibility, affecting range of motion
- Swelling or tenderness around inflamed joints
- Popping or crackling noises or a sensation of grating when using the affected joint
A Review of Treatments

Good nutrition, regular exercise, and certain medications can help you manage living with osteoporosis and/or osteoarthritis.
Osteoporosis Treatments
Osteoporosis is preventable, treatable, and manageable.
Osteoporosis treatments include:
- Sufficient calcium intake: A diet rich in calcium will go a long way to keep your bones strong and healthy.
- Regular weight-bearing exercise: Walking, jogging, dancing, and lifting weights make your muscles work against gravity and strengthen your bones.
- Curb alcohol and caffeine consumption. Alcohol affects how your body absorbs calcium and Vitamin D. Caffeine saps calcium from bones, which weakens them.
- Do not smoke. If you don’t smoke, don’t start. If you do, the best course of action for healthy bones is to stop smoking.
In addition to the preventive measures listed above, treatment of established osteoporosis may include medications. Your Moreland OB-GYN provider will work with you to determine the course of medication that works best for you.
If you’re living with osteoporosis, additional courses of action for you are :
- Preventing falls: Set up your living environment inside and outside your home to keep you safe from falls. Keep walking paths clear of clutter like rugs, computer or television cables, and electric cords. Make sure your lighting is bright and allows you to see where you’re stepping. Equip your bathroom with grab bars and use them. Make sure stair rails are secure and use them to climb up and down stairs. Wear sensible shoes. Use a cane, if necessary, to steady yourself.
- Strengthening your balance: A daily exercise routine can help reduce your risk of falling. Gentle yoga and tai chi are great routines to help improve or maintain your balance. Physical therapy may be prescribed to help evaluate and properly instruct you through an exercise program to help you improve balance.
Osteoarthritis Treatments
While you can’t reverse osteoarthritis, you can manage it with:
- Medication: Doctor-recommended doses of acetaminophen products and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen sodium can help with pain. Taking more than recommended may cause damage to certain internal organs. Topical NSAIDs are also available to treat joint pain with fewer harmful side effects. Your doctor may prescribe duloxetine, normally used as an antidepressant, to help relieve pain caused by osteoarthritis.
- Therapy: Your doctor may prescribe physical therapy to reduce pain by strengthening muscles around the affected joints.
- Surgical and other medical procedures: Cortisone injections into the joint may bring temporary relief, but the number of injections is limited to 3 or 4 per year. Bone realignment for knees and joint replacement for hips and knees are options for worn-out joints.
- Lifestyle alterations: Adding low-impact exercise like walking, bicycling, and swimming can strengthen muscles around your joints and help stabilize them. Consult with your doctor before you begin a new exercise routine. Losing weight can reduce stress on weight-bearing joints. According to the Arthritis Foundation, being just 10 pounds overweight puts an extra 15 to 50 pounds of pressure on your knees. Discuss a weight-loss plan with your doctor before beginning one.
When to See Your Moreland OB-GYN
Although you can’t stop aging, you can take steps to reduce the effects of osteoporosis and osteoarthritis.
Step one, contact your Moreland provider. Have a conversation about your concerns—whether it’s symptoms you’re currently experiencing or a genetic predisposition that makes you apprehensive about your future.
Your Moreland provider can help lead you to better health! Request your appointment online today.